When our kids were about 2, I got a terrifying email from a mom-friend. During dinner, Carrie suddenly noticed that her son wasn’t speaking. “His face was starting to turn blue, and he lost consciousness,” she later told me. “I yelled to my husband, “He’s choking he’s choking!” and ran to my phone and called 911.” While 911 gave instructions that Carrie was able to yell out to her husband, she felt terrified. “I remember thinking, Oh my god, I’m watching my son die. I’m watching my 2 year old son die. This can’t be happening.” Her husband performed a few rounds of back blows while her son lay there unconscious, and ultimately they dislodged the food as paramedics were arriving. “My son was fine, apart from a sore throat and red/bruised back from the back blows,” Carrie says, adding that after her son was evaluated and released from the hospital, the doctors told her that he would not have survived had it not been for the CPR administered by her husband.
CPR is really important. If you can, sign up for a class, because seeing it done and practicing it in person makes a huge difference. Whether or not you are able to take a CPR training course, there are some specific steps to take when performing CPR on an infant or child. First of all, it is important to know if your child actually needs CPR, or if he or she is alert but choking. “The first, and most important distinction between a choking event and a CPR event, is whether or not an infant or a child is responsive,” says Vanessa Anton, a CPR certified instructor and founder of Common Sense CPR in New York City. “A responsive infant or child is in obvious distress. An unresponsive infant or child is just that – unresponsive.” Only an unconscious or unresponsive child needs CPR. If the child is distressed or changing color but still responsive, they are actively choking and do not need cardiopulmonary resuscitation. However, if your baby or child has lost consciousness, that is when it is time to administer CPR by performing the following steps.
1. Check the scene. Look around and make sure you’re not underneath a falling object or in the road or something. You can’t help if you get hurt, too.
2. Check for responsiveness. Tickle the bottoms of your baby’s feet or tap a toddler’s shoulder to see if they respond.
3. Find a flat surface. IF your baby does not respond, place him on a flat surface, such as a table or the floor.
4. Check airways. Look at and listen to the baby’s bare chest for 5-10 seconds to make sure he is not breathing. “We are looking for rise and fall of the chest, discoloration, restrictions, bruises, cuts, allergic reactions,” says Anton.
5. Call 911. IF your baby is definitely breathing, immediately call 911. If someone else is with you, have them call 911. If you are alone and your baby is either not breathing, or having trouble (or you’re not sure), perform CPR before calling 911.
6. Begin CPR.
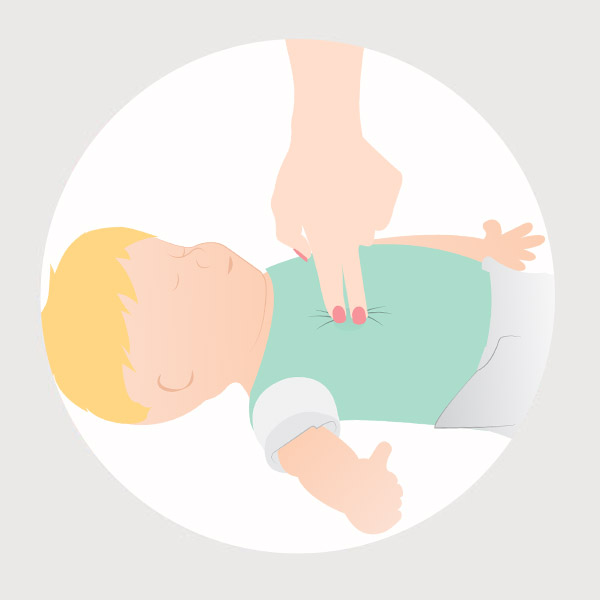
How to Do CPR on Babies (up to age 1)

- Place two fingers vertically in the middle of the baby’s chest along the horizontal line of the nipples (try to avoid pressing the lower tip of the sternum).

- Press into the chest (about 1.5 inches deep), for 30 compressions at a rate of between 100-120 compressions per minute (roughly every other second).

- After 30 compressions, lift the baby’s chin, cover his nose and mouth with your mouth and attempt 2 small breaths. If the baby’s chest rises, give another breath, but if there is no response, resume with another 30 compressions followed by 2 breaths. Continue CPR until the infant responds, someone else takes over, or the scene becomes unsafe. “These are the only reasons to stop,” says Anton. “People have received CPR for over an hour and been resuscitated, it works.”
How to Do CPR on Children (ages 1 to 8)
There are two main differences in administering CPR in toddlers and children vs. babies:
- Place the heal of one palm in the middle of the chest along the horizontal line of the nipples, once again avoiding the lower tip of the sternum).

- Press into the chest (about 2 inches deep), for 30 compressions at a rate of between 100-120 compressions per minute (roughly every other second).
CPR sources: American Red Cross and Vanessa Anton, a CPR certified instructor and founder of Common Sense CPR